A brief guide to the ileo-anal pouch (Restorative Proctocolectomy)
Despite modern medical treatment up to a third of patients with ulcerative colitis will eventually require surgery during their lifetime. Three operations are available including conventional proctocolectomy, restorative proctocolectomy with ileal pouch-anal anastomosis and colectomy with ileorectal anastomosis (IRA). The last of these is only suitable for the few patients whose rectum is relatively free of inflammation and where there is no dysplasia (pre-cancerous changes) or established cancer in the large bowel –this is uncommon.
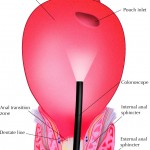
Conventional proctocolectomy leaves the patient with a permanent ileostomy (bag) which most patients wish to avoid. Restorative proctocolectomy or ‘the pouch operation` was described by Sir Alan Parkes and Professor John Nicholls in 1978 and is accepted as the operation of choice for patients with ulcerative colitis who require surgery.
What can be expected after restorative proctocolectomy?
It is important to appreciate that bowel function will not be ‘normal’ after surgery. The advantages of this operation compared to conventional proctocolectomy are;
(i). Patients are able to use the toilet in the normal way –this means that patients do not need to carry stoma equipment with them on their travels.
(ii). Urgency (the need to find a toilet quickly) –which is probably the most disabling symptom of ulcerative colitis is removed.
(iii). Cosmetic –a permanent stoma (bag) is avoided.
Normal pouch function
-Patients should expect to open their bowels an average of 6-8 times in each 24hr period, about half of all patients will need to use the toilet over night.
-Patients should be able to ‘hold-on’ for 1 hour.
Fertility after surgery
In female patients fertility is halved after pouch surgery. Importantly fertility is also halved after conventional pan-proctocolectomy (ie. removal of the colon and rectum). This reduction in fertility can be avoided by undergoing a subtotal colectomy (the usual operation performed as an emergency in acute severe ulcerative colitis) and not having the rectum removed until after the patient has had her children.
This reduction is fertility is due to ulcerative colitis itself but also pelvic surgery where adhesions form around the fallopian tubes.
Importantly studies have shown that IVF treatment is very effective in pouch patients who are having difficulty conceiving.
Do patients need regular endoscopic examination of their pouch after surgery?
The majority of patients do not need endoscopic surveillance. Only those patients who had evidence of pre-cancer (dysplasia) or cancer of the large bowel at the time of surgery or who have Primary Sclerosing Cholangitis (PSC) or have chronic pouchitis require regular (once per year) endoscopic examination.
How long do pouches last?
The majority of pouches last for life.
After 20 years 10-15% of patients will no longer have a functioning pouch
What are the causes of pouch failure?
The top three causes of pouch failure are:
(i). Pelvic sepsis –infection developing due to a leak at the join between the pouch and the anal canal.
(ii). Poor pouch function –the pouch simply doesn’t work very well
(iii). Chronic pouchitis